Welcome to Preceptorship!
This is our dedicated page to all things Preceptorship. Below you will find all the resources and information you may need. Please don’t hesitate to reach out for more information from our Preceptorship lead if cant find what you are looking for. To get you started please watch the video below to learn about what a Preceptorship is.
What is Preceptorship?
The purpose of preceptorship is to provide support, guidance and development for all newly registered and new to practice practitioners to build confidence and competence as they transition from student to autonomous professional or from a previous sector into primary care (NHSE “National Preceptorship Project for Nursing” – June 2022)
The NHSE Long Term Workforce Plan (NHSE 2023) recognises that good quality preceptorship is one of the key principles in recruitment, integration and transitional roles and staff retention, with its “train, retain, reform” strategic challenges.
The plan states that ‘scaling of NHS care delivered in the community requires rapid expansion of the necessary workforce and the development of more flexible and integrated teams,’ which encourages practices to fully support preceptorship in the integration of AHP roles, finding new ways of working in Primary Care areas.
The Plan’s aim to increase training places for Allied Health Professions (AHPs) and other professional groups, indicates that a robust preceptorship support should be in place once they join Primary Care, to ensure they experience a positive environment and welcoming culture.
Therefore, our Preceptorship Programme is available for all professions working within primary care.
Investment in preceptorship provides triple returns: it improves retention, it increases skills and confidence, and it produces economic value (NHSE, 2022). It also ensures patient safety, stability and satisfaction with their local Primary Care services.
Preceptorship is not a replacement for basic induction or mandatory training. It involves commitment from the Practice, utilising experienced Practitioners in preceptorship roles for the first 6-12 months of new-to-practice practitioners commencing employment.
The National Preceptorship Framework programme is intended for all Trusts and organisations to support newly qualified and new-to-practice practitioners. It is expected that the basic National Preceptorship core standards are to have been achieved by September 2023, with organisations aiming for the gold standards thereafter.
In order for the Lancashire and South Cumbria Primary Care Training Hub to effectively support preceptorship in the General Practices in the area, we have identified from a scoping exercise that there is a need for promotion of preceptorship in practice and LSCTH are endeavouring to provide the support required for implementation.
References:
NHSE Ten Point Action Plan for General Practice Nursing (2017)
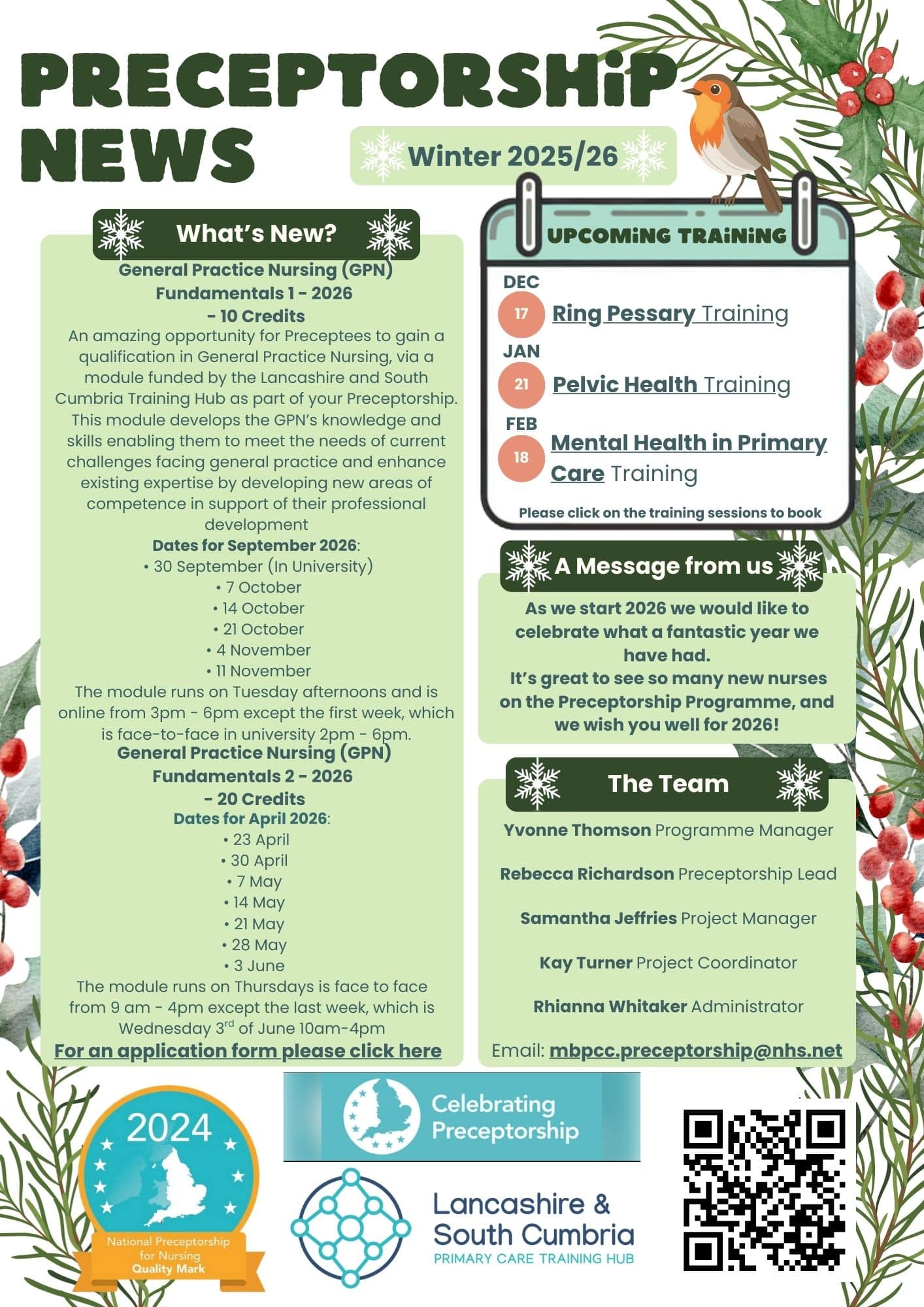
Celebrating Preceptorship

Lancashire & South Cumbria Primary Care Training Hub are pleased to announce that they have been awarded the Gold Standard Quality Mark for Preceptorship from February 2024.
This is a prestigious award that can be shared with all practices who engage in the preceptorship programme. Practices that engage with the Preceptorship Programme can display this Quality mark on Social channels, the Practice’s website and Email signatures to showcase participation in Preceptorship.
Recent Feedback
‘Stepping into primary care from a busy secondary care environment was a huge change for me, especially having never have worked in primary care before, other than as a nursing student. The preceptorship programme ensured I received all relevant training in a timely manner and was supported in doing so. I have always had a point of contact, both in practice and from the learning hub if I had any questions or felt I needed extra training.’ Rebecca Gee, Practice Nurse, August 2025.

Where does Preceptorship sit?
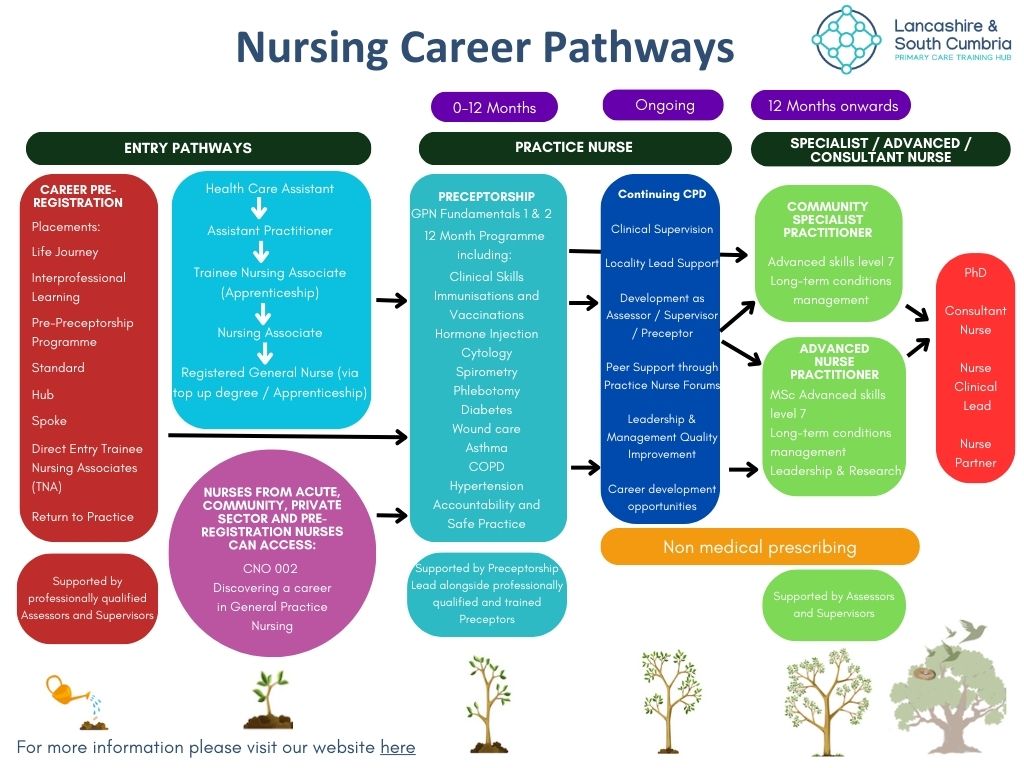
Preceptorship is part of the Nursing Career Pathway and when adopted offers a multitude of benefits for the Preceptee, the Preceptor and the Practice.
What's Available to Support?

For The Preceptee:
- Preceptor
- Handbook
- Fundamentals Module (for GPN’s only)
- Red Whale
- Cytology Training
- Spirometry
- Immunisation and Vaccination Training
- Venupuncture Training
- Peer Support
- Training Hub offers
- Support from members of the Training Tub team
- Support with CPD
Fundamentals Application Form
FUNDAMENTALS 1:
Timetable September 2026
Dates and Information
FUNDAMENTALS 2:
Timetable April 2026

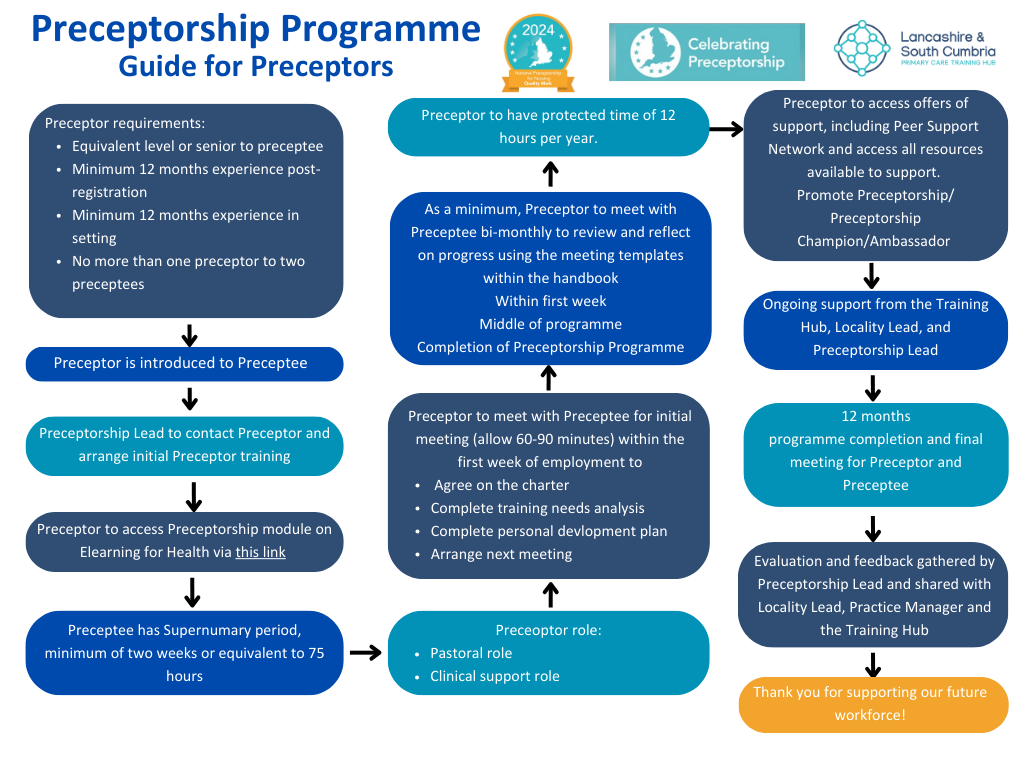
For The Preceptor:
- Initial Training which includes:
- An in-depth look at the national preceptorship programme
- An explanation of the roles, responsibilities and skills of the preceptor
- Guidance on how preceptors can support preceptees in practice
- An explanation on how to complete the required documentation
- The development of peer preceptorship support networks
- Peer support Network
- Access to Mentor Support Sessions
- Clinical Supervision Sessions
- ELearning for Health (Preceptor Compendium)
- Protected time
- Ongoing support from the Training Hub and Preceptorship Lead
Additional Methods of Support:
LSC system preceptorship sessions which the LSC AHP Workforce Programme Team have on offer to support current preceptees and people who have completed the course within the last year:
- Lancashire and South Cumbria Local and National Nurse and AHP Quarterly Update Forums – Lancashire and South Cumbria Training Hub offer a Local Nurse and AHP Quarterly Update Forum – please join the forum to keep up to date with recent recommendations to practice and link with other nurses in other localities.
- An introduction to the Lancashire and South Cumbria Integrated Care Board & ICB AHP Workforce Team
These sessions are open to all professions. There will be a rolling programme for these session with them running twice a year. The team are also looking at running these sessions for all staff to access, information on these sessions and dates will come out in due course

Resources for all staff within Primary Care
Spotlight on Knowledge for Healthcare
Meet the Team
We have a fantastic team to support the Preceptorship Programme. If you have any questions or queries, please feel welcome to reach out to us and we will help to support you the best way we can.

Rebecca Richardson
Preceptorship Lead
About Rebecca

Yvonne Thomson
Programme Lead
About Yvonne
A Registered General Nurse, who has completed the ILM Coaching qualification with a multi-faceted career spanning over nearly 30 years. Experience has been gained within the Armed Forces and the NHS across secondary care, community, and Primary Care. Strategic and operational leadership, management, education, service development and re design, alongside project management expertise has been achieved throughout my career. Passionate about educational and career development and really enjoys working with people to develop their own skills and knowledge within a coaching and mentoring ethos.

Samantha Jefferies
Project Manager (Placements)
About Sam
I am the Project Manager for Lancashire & South Cumbria Primary Care Training Hub, for Placements.
Working in partnership with the Five Training Hub Localities;
Providing support to each Locality Training hub, Leads, Operation Managers, General Practice Education Facilitators (GPEFs), Trainee Nursing Associate Practice Education Facilitators (TNA PEFs), and organisation Practice Education Facilitators (PEFs) in expanding clinical placements and ensuring the provisions are of a high-quality multi-professional learning environment across the sectors.

Kay Turner
Project Co-ordinator
About Kay
Highly qualified and experienced in all aspects of administration, recruitment, human resources and leadership, spanning over more than 40 years. Kay’s previous roles include Personal Legal Secretary; Director and Business owner of a Management Consultancy; Headteacher’s Personal Assistant; Human Resources Manager; Office Manager and Business Owner of a small hand-made jewellery organisation. Having supported learners in an educational setting for over 23 years, supporting career development within the NHS has allowed Kay to continue to support the next generation workforce. Enthusiastic about supporting others to achieve their potential Kay has a zest for learning and embraces new ideas and concepts.

Rhianna Whitaker
Administrator
About Rhianna
Rhianna is new and excited to provide support to the preceptorship team. She has 4 years experience in legal and aerospace administration. she gained experience in procurement, safety, and data management.
Rhianna has a Masters degree in Speech and Language Therapy and is also pursuing this as a career. She is hoping to specialise into voice therapy and clients with neurological conditions. During her studies in the pandemic Rhianna worked first hand with both clinicians and clients, her dissertation was on clinical supervision during COVID-19.
Benefits For The Practice
The Lancashire & South Cumbria Primary Care Training hub has a Preceptorship Lead who can support individual practices with their preceptorship plan. Please contact [email protected] for more details.
see the section below, Useful Links and Resources: we have put together the links you may need to start your preceptorship policy, a guide to what is expected from practices, and the allocated timeframes recommended for new professionals to have in their preceptorship period.
The benefits of Preceptorship for the practice:
Improved Confidence and Competence in New Nurses
- Structured support helps new nurses transition smoothly into general practice roles.
- Builds clinical skills, communication, decision-making, and understanding of primary care.
- Reduces anxiety and uncertainty, especially for newly qualified nurses or those new to primary care
Professional Development and Career Pathways
- Encourages mentorship, collaboration, and knowledge-sharing between experienced and newer staff.
- Fosters a culture of learning and professional development within the practice.
- Preceptorship provides a clear developmental framework for new nurses.
- Practices that invest in staff development attract high-calibre candidates.
Practice Reputation and Quality Standards
- Shows commitment to excellence in training and support.
- Helps meet CQC expectations for workforce development and safe care.
- Quality Mark shared with all Practices that engage with the Preceptorship to share on the practice’s website and social channels
Enhanced Retention and Reduced Turnover
- Nurses who feel supported are more likely to stay in the role and within the practice.
- Reduces recruitment costs and the disruption of frequent staff changes.
Better Patient Care and Safety
- Well-supported nurses are more confident, competent, and less likely to make errors.
- Patients benefit from more consistent, knowledgeable care.
Supports Diversification of the Workforce
- Makes general practice more accessible to a broader range of nurses, including those transitioning from secondary care or returning to practice.
Benefits for the Preceptor

The Preceptorship programme offers a multitude of benefits for the Preceptors supporting Preceptees.
- Access to eLearning for Health Preceptor Compendium
- Peer support sessions
- Support from Preceptorship Lead
- One-to-one training to establish the roles and responsibilities of being a Preceptor
- Protected time to prepare for supporting Preceptee
- Mentor support sessions to support coaching techniques
Contributing to the Future of Nursing
- Helps shape the next generation of primary care nurses.
- Contributes to the sustainability and resilience of the nursing workforce
Personal Growth and Confidence
- Supporting others can build confidence in one’s own abilities.
- Encourages reflection on past challenges and successes.
Recognition and Value
- Demonstrates expertise and commitment to the profession.
- May lead to formal recognition, enhanced credibility, or further opportunities within the practice or local training hubs.
Reinforcement of Own Knowledge
- Teaching others encourages reflection on one’s own practice.
- Clarifying procedures or explaining clinical reasoning can refresh and deepen personal knowledge.
Enhanced Job Satisfaction
- Many preceptors find mentoring deeply rewarding.
- Seeing a new nurse grow in confidence and skill can boost morale and job fulfilment.
Professional Development and Leadership Skills
- Builds leadership, teaching, and mentoring skills.
- Enhances communication, delegation, and feedback-giving abilities.
- Looks great on a CV—especially for career progression into senior roles or advanced practice.
Benefits For The Preceptee

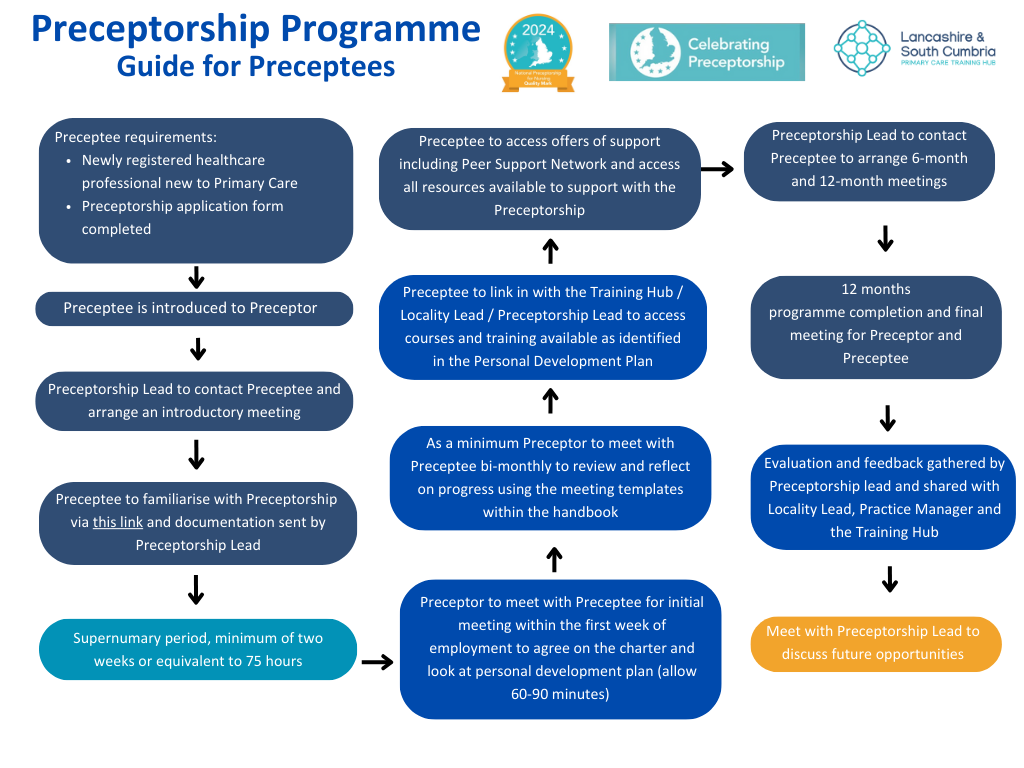
L&SC PCTH preceptorship programme you will receive a copy of our comprehensive e-handbook to work through with your preceptor.
You will have regular meetings with an allocated Preceptor to complete a training needs analysis and a learning and development plan. As part of the preceptorship programme you will have access to multiple courses and training opportunities to broaden your knowledge and skills.
Some examples are:
- Cytology training
- Immunisations and Vaccinations
- Spirometry
- Access to Red Whale
- GPN Fundamentals (for GPNs only)
- Peer support sessions
- Handbook
- Clinical skills
- Phlebotomy
- Chronic Disease Management
Develops Clinical and Non-Clinical Skills
- Exposure to a wide range of skills specific to general practice.
- Enhances time management, documentation, and communication.
Provides a Safe Space to Learn
- You can ask questions and seek guidance without fear of judgment.
- Encourages reflection and learning from real-life scenarios
Promotes Professional and Emotional Support
- Reduces stress, anxiety, and feelings of isolation.
- Offers mentorship and emotional encouragement from an experienced nurse.
Improves Patient Care
- Supported nurses are more likely to deliver safe, effective, and compassionate care.
- Encourages a patient-centred approach right from the start.
Encourages Long-Term Career Development
- Introduces the nurse to career pathways within primary care.
- Instills a commitment to lifelong learning and professional growth.
Improves Job Satisfaction and Retention
- Nurses who feel supported are more likely to stay in their role and build a long-term career in general practice.
Pastoral Support
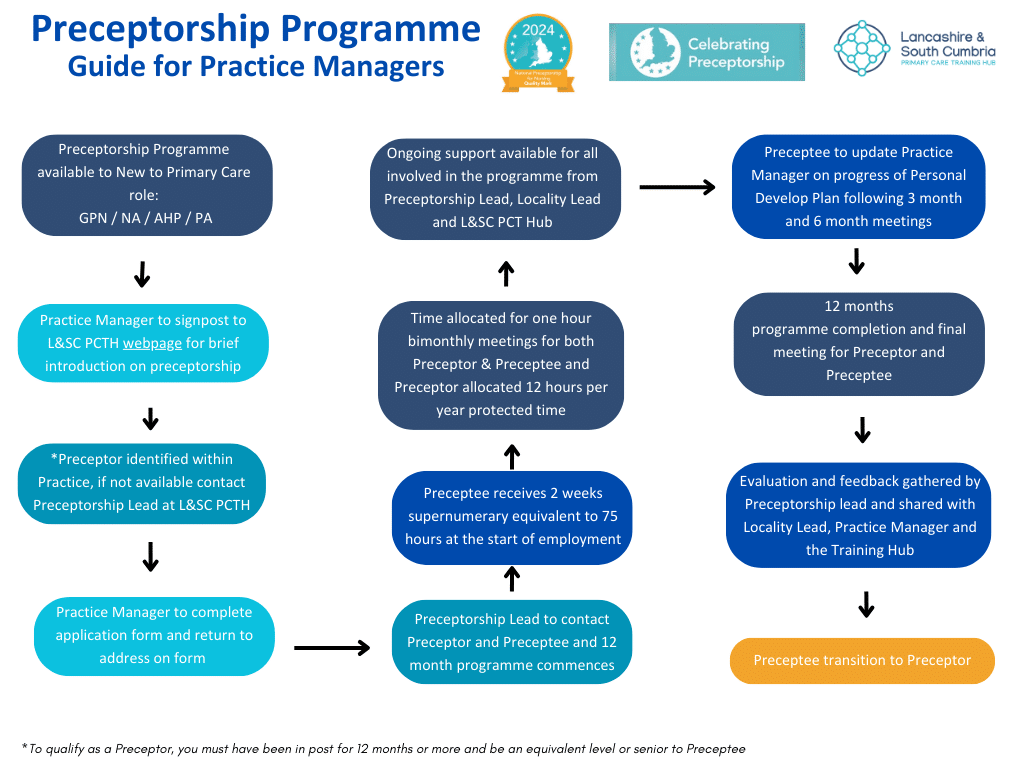
How to access Preceptorship
All that’s required is a simple application form to be filled in by the practice manager, Preceptor, or the Preceptee.
Please email [email protected] or [email protected] for a copy of the application form; once you have completed the application form please return it to Kay or Rhianna.
All that’s required is a simple application form to be filled in by the practice manager, Preceptor, or the Preceptee.
Please email [email protected] or [email protected] for a copy of the application form; once you have completed the application form please return it to Kay or Rhianna.
Resources
Useful Links and Resources
Guidance and Information for all HCPs
Click here to view this document
Click here to view this document
Click here to view this document
Click here to view this document
Click here to view this document
Click here to view this document
A new National Induction Framework is now available for all new joiners of health and social care and which delivers on the first recommendation from the Messenger review to create an entry-level induction for all new joiners of health and social care. There are helpful guides and templates for recruiting managers to support new joiners. You will need to register for an account with the Leadership Academy to access.
Click here to view Document
Find all Health and Wellbeing helplines, training, opportunities and resources here.
Click here to view this document
Click here to view this document
For Preceptors
Click here to view this document
Click here to view this document
For General Practice Nurses
Click here to view this document
Click here to iew this document
Click here to view this document
The Frameworks provides a standard and greater clarity on the scope of practice for nurses working within primary care and general practice settings.
Click here to view this document
For Allied Health Professionals
For Physician Associates
GPN Educational Resources
Diabetes Educational Resources for General Practice and Primary Care Nurses
it is vital that GPNs are up to date with information on diabetes and work with patients to maximise their health with health education and promotion.
Type 1 diabetes is an autoimmune condition where by the pancreas does not produce insulin and the treatment is always insulin. Multiple daily insulin injections are used by many but the used of insulin pumps and hybrid closed loop systems are increasing.
• Type 2 diabetes occurs due to insulin resistance and the insulin produced by the pancreas doesn’t work effectively. Over time insufficient insulin production may also occur. Type 2 diabetes accounts for around 10% of the annual NHS budget.
• Gestational diabetes (GDM) occurs during pregnancy and increases the risk of developing type 2 diabetes after pregnancy. Women with previous GDM should have annual HbA1c surveillance.
• Type 3c, MODY and Latent Autoimmune Diabetes in Adults (LADA) are less common types of diabetes but may still be seen in general practice.
Heart Failure Core Career and Capability Framework
Heart failure is the destination condition of most cardiovascular diseases.
An estimated 1 million people are living with heart failure in the UK. There are 200,000 new diagnoses each year with an estimated 400,000 cases currently undetected in UK.
80% of Heart Failure first diagnoses as made as emergency admissions to hospital, with several patients visiting their GPs with symptoms in the months before admission.
Menopause Educational Resources for General Practice nurses
The menopause usually affects women between the ages of 45 and 55, but it can happen earlier for reasons such as surgery to remove the ovaries or the uterus, or because of cancer treatments like chemotherapy.
Although each person will experience the menopause in a different way, three out of four people going through the menopause will experience symptoms, and for one in four, these will be severe and impact their day-to-day life.
Symptoms can last for several years and can include anxiety, low mood, hot flushes, difficulty concentrating, headaches, and insomnia.
Wound Care Educational Resources for Community and Primary Care Nurses
Wound care should not be viewed as a separate clinical issue but as an integral part of the holistic assessment, including optimisation of long-term conditions which cause or contribute to wounding and delayed/non-healing.
Failure to diagnose wound type, leads to potential delays in providing patients with appropriate evidence-based treatment pathways, which could result in delayed/non healing and/or secondary complications.
Affecting 1:11, asthma is the most common long-term condition in children and young people (CYP). It can be wrongly perceived as a mild disease, and research shows that it is often not taken seriously enough. Those with ‘mild asthma’ can deteriorate, causing increased morbidity and mortality.
Education for children and their families, clinicians and wider members of health care teams about recognising and managing triggers, symptoms and asthma attacks is key to effective asthma control.
Although some asthma attacks come on without warning, many build up slowly, over hours to days. This means that there is often a window of opportunity to treat them in primary care before symptoms escalate into an emergency.
Patients must be educated to understand their triggers and
how they can avoid or manage them.
Patients must know the signs of worsening asthma so they can get early help.
Cancer Educational Resources for General Practice and Primary Care Nurses
The NHS ambition in the Long -Term Plan is to diagnose 75% of cancers at stage I or II by 2028. Earlier diagnosis means cancers are easier to treat and result in better patient outcomes.
There are increasing numbers of people living with cancer in the United Kingdom due to increased survival and an ageing population.
There are 393,000 new cancer diagnosis each year, this is expected to be 500,000 annually by 2040.
Minor illness Core Career and Capability Framework
This accounts for a significant proportion of primary care presentations. Conditions such as coughs, colds, sore throats, ear infections, mild gastrointestinal issues, and skin complaints are among the most common reasons people seek primary care support.
An estimated 20–40% of GP consultations are related to minor illness. Many of these conditions are self-limiting and could be safely managed at home with appropriate self-care advice. However, minor illness still contributes to unnecessary demand on general practice and emergency departments, with millions of potentially avoidable appointments each year.